Many of the problems confronting health professionals today are of extreme importance to the engineer because they involve the fundamental aspects of device and systems analysis, design, and practical application—all of which lie at the heart of processes that are fundamental to engineering practice. These medically relevant design problems can range from very complex large-scale constructs, such as hospital information systems, to the creation of relatively small and “simple” devices, such as recording electrodes and transducers used to monitor the activity of specific physiological processes.
The American health care system, therefore, encompasses many problems that represent challenges to certain members of the engineering profession, called biomedical engineers. Since biomedical engineering involves applying the concepts, knowledge, and approaches of virtually all engineering disciplines (e.g., electrical, mechanical, and chemical engineering) to solve specific health care–related problems, the opportunities for interaction between engineers and health care professionals are many and varied.
Although what is included in the field of biomedical engineering is considered by many to be quite clear, many conflicting opinions concerning the field can be traced to disagreements about its definition. For example, consider the terms biomedical engineering, bioengineering, biological engineering, and clinical (or medical) engineer, which are defined in the Bioengineering Education Directory. While Pacella defined bioengineering as the broad umbrella term used to describe this entire field, bioengineering is usually defined as a basic-research oriented activity closely related to biotechnology and genetic engineering—that is, the modification of animal or plant cells or parts of cells to improve plants or animals or to develop new microorganisms for beneficial ends. In the food industry, for example, this has meant the improvement of strains of yeast for fermentation. In agriculture, bioengineers may be concerned with the improvement of crop yields by treatment plants with organisms to reduce frost damage. It is clear that bioengineers for the future will have tremendous impact on the quality of human life. The full potential of this specialty is difficult to image. Typical pursuits include the following:
• The development of improved species of plants and animals for food production
• The invention of new medical diagnostic tests for diseases
• The production of synthetic vaccines from clone cells
• Bioenvironmental engineering to protect human, animal, and plant life from toxicants and pollutants
• The study of protein-surface interactions
• Modelling of the growth kinetics of yeast and hybridoma cells
• Research in immobilized enzyme technology
• The development of therapeutic proteins and monoclonal antibodies
The term biomedical engineering appears to have the most comprehensive meaning. Biomedical engineers apply electrical, chemical, optical, mechanical, and other engineering principles to understand, modify, or control biological (i.e., human and animal) systems. When a biomedical engineer works within a hospital or clinic, he or she is more properly called a clinical engineer. However, this theoretical distinction is not always observed in practice, since many professionals working within U.S. hospitals today continue to be called biomedical engineers.
The breadth of activity of biomedical engineers is significant. The field has moved significantly from being concerned primarily with the development of medical devices in the 1950s and 1960s to include a more wide-ranging set of activities. As shown in Figure 1.9, the field of biomedical engineering now includes many new career areas:
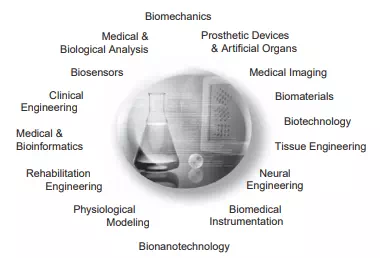
FIGURE 1.9 The world of biomedical engineering.
• Application of engineering system analysis (physiologic modelling, simulation, and control to biological problems)
• Detection, measurement, and monitoring of physiologic signals (i.e., biosensors and biomedical instrumentation)
• Diagnostic interpretation via signal-processing techniques of bioelectric data
• Therapeutic and rehabilitation procedures and devices (rehabilitation engineering) • Devices for replacement or augmentation of bodily functions (artificial organs)
• Computer analysis of patient-related data and clinical decision making (i.e., medical informatics and artificial intelligence)
• Medical imaging—that is, the graphical display of anatomic detail or physiologic function
• The creation of new biologic products (i.e., biotechnology and tissue engineering) Typical pursuits of biomedical engineers include the following:
• Research in new materials for implanted artificial organs
• Development of new diagnostic instruments for blood analysis
• Writing software for analysis of medical research data
• Analysis of medical device hazards for safety and efficacy
• Development of new diagnostic imaging systems
• Design of telemetry systems for patient monitoring
• Design of biomedical sensors
• Development of expert systems for diagnosis and treatment of diseases
• Design of closed-loop control systems for drug administration
• Modelling of the physiologic systems of the human body
• Design of instrumentation for sports medicine
• Development of new dental materials
• Design of communication aids for individuals with disabilities Study of pulmonary fluid dynamics
• Study of biomechanics of the human body
• Development of material to be used as replacement for human skin
The preceding list is not intended to be all-inclusive. Many other applications use the talents and skills of the biomedical engineer. In fact, the list of activities of biomedical engineers depends on the medical environment in which they work. This is especially true for the clinical engineers—biomedical engineers employed in hospitals or clinical settings. Clinical engineers are essentially responsible for all the high-technology instruments and systems used in hospitals today, the training of medical personnel in equipment safety, and the design, selection, and use of technology to deliver safe and effective health care.
Engineers were first encouraged to enter the clinical scene during the late 1960s in response to concerns about electrical safety of hospital patients. This safety scare reached its peak when consumer activists, most notably Ralph Nader, claimed, “At the very least, 1,200 Americans are electrocuted annually during routine diagnostic and therapeutic procedures in hospitals.” This concern was based primarily on the supposition that catheterized patients with a low-resistance conducting pathway from outside the body into blood vessels near the heart could be electrocuted by voltage differences well below the normal level of sensation. Despite the lack of statistical evidence to substantiate these claims, this outcry served to raise the level of consciousness of health care professionals with respect to the safe use of medical devices.
In response to this concern, a new industry—hospital electrical safety—arose almost overnight. Organizations such as the National Fire Protection Association (NFPA) wrote standards addressing electrical safety specifically for hospitals. Electrical safety analyser manufacturers and equipment safety consultants became eager to serve the needs of various hospitals that wanted to provide a “safety fix” and of some companies, particularly those specializing in power distribution systems (most notably isolation transformers). To alleviate these fears, the Joint Commission on the Accreditation of Healthcare Organizations (then known as the Joint Commission on Accreditation of Hospitals) turned to NFPA codes as the standard for electrical safety and further specified that hospitals must inspect all equipment used on or near a patient for electrical safety at least every six months. To meet this new requirement, hospital administrators considered a number of options, including (1) paying medical device manufacturers to perform these electrical safety inspections, (2) contracting for the services of shared-services organizations, or (3) providing these services with in-house staff. When faced with this decision, most large hospitals opted for in-house service and created whole departments to provide the technological support necessary to address these electrical safety concerns.
As a result, a new engineering discipline—clinical engineering—was born. Many hospitals established centralized clinical engineering departments. Once these departments were in place, however, it soon became obvious that electrical safety failures represented only a small part of the overall problem posed by the presence of medical equipment in the clinical environment. At the time, this equipment was neither totally understood nor properly maintained. Simple visual inspections often revealed broken knobs, frayed wires, and even evidence of liquid spills. Many devices did not perform in accordance with manufacturers’ specifications and were not maintained in accordance with manufacturers’ recommendations. In short, electrical safety problems were only the tip of the iceberg. By the mid-1970s, complete performance inspections before and after equipment use became the norm, and sensible inspection procedures were developed. In the process, these clinical engineering pioneers began to play a more substantial role within the hospital. As new members of the hospital team, they did the following:
• Became actively involved in developing cost-effective approaches for using medical technology
• Provided hospital administrators with advice regarding the purchase of medical equipment based on their ability to meet specific technical specifications
• Started using modern scientific methods and working with standards-writing organizations
• Became involved in the training of health care personnel regarding the safe and efficient use of medical equipment
Then, during the 1970s and 1980s, a major expansion of clinical engineering occurred, primarily due to the following events:
• The Veterans Administration (VA), convinced that clinical engineers were vital to the overall operation of the VA hospital system, divided the country into biomedical engineering districts, with a chief biomedical engineer overseeing all engineering activities in the hospitals in that district.
• Throughout the United States, clinical engineering departments were established in most large medical centres and hospitals and in some smaller clinical facilities with at least three hundred beds.
• Health care professionals—physicians and nurses—needed assistance in utilizing existing technology and incorporating new innovations.
• Certification of clinical engineers became a reality to ensure the continued competence of practicing clinical engineers.
During the 1990s, the evaluation of clinical engineering as a profession continued with the establishment of the American College of Clinical Engineering (ACCE) and the Clinical Engineering Division within the International Federation of Medical and Biological Engineering (IFMBE). Clinical engineers today provide extensive engineering services for the clinical staff and serve as a significant resource for the entire hospital (Figure 1.10). Possessing in-depth knowledge regarding available in-house technological capabilities as well as the technical resources available from outside firms, the modern clinical engineer enables the hospital to make effective and efficient use of most if not all of its technological resources.
Biomedical engineering is thus an interdisciplinary branch of engineering heavily based in both engineering and the life sciences. It ranges from theoretical, nonexperimental undertakings to state-of-the-art applications. It can encompass research, development, implementation, and operation. Accordingly, like medical practice itself, it is unlikely that any single person can acquire expertise that encompasses the entire field. As a result, there has been an explosion of biomedical engineering specialties to cover this broad field. Yet, because of the interdisciplinary nature of this activity, there are considerable interplay and overlapping of interest and effort between them. For example, biomedical engineers engaged in the
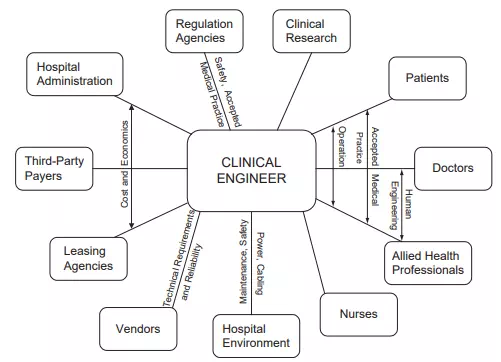
FIGURE 1.10 The range of interactions that a clinical engineer may be required to engage in a hospital setting.
development of biosensors may interact with those interested in prosthetic devices to develop a means to detect and use the same bioelectric signal to power a prosthetic device. Those engaged in automating the clinical chemistry laboratory may collaborate with those developing expert systems to assist clinicians in making clinical decisions based upon specific laboratory data. The possibilities are endless.
Perhaps an even greater benefit of the utilization of biomedical engineers lies in the potential for implementing existing technologies to identify and solve problems within our present health care system. Consequently, the field of biomedical engineering offers hope in the continuing battle to provide high-quality health care at a reasonable cost. If properly directed toward solving problems related to preventative medical approaches, ambulatory care services, and the like, biomedical engineers can provide the tools and techniques to make our health care system more effective and efficient.

Comments are closed.