A few years ago, Bryan Pukenas, MD, learned something old that led him to something new.
The “something old” was a technique that had fallen out of fashion many decades ago in Pukenas’ specialty, interventional neuroradiology. It’s called a suboccipital puncture, and it’s a method of injecting a needle directly into the fluid surrounding the base of the brain. It was widely performed in the 1920s and 1930s as a way to extract cerebrospinal fluid, but due to some safety concerns that arose at that time, other methods began to supersede it. Now, more often, cerebrospinal fluid is extracted through a lumbar puncture in the lower back, for instance
But the suboccipital puncture came back to Penn thanks to prompting by Penn Gene Therapy Program Director James Wilson, MD, PhD, who had a good reason for asking: Gene therapies that his team and others developed had been moving rapidly toward greater use in patients, both in clinical trials and in the form of FDA-approved therapies. For many of these therapies, including a new therapy for spinal muscular atrophy, Zolgensma, the therapeutic genes are intended to reach a target inside the brain. But how to get them there?
In pre-clinical studies, researchers in the lab found that injecting the gene vector into the suboccipital space led to 10 to 100 times more of the therapeutic gene reaching the body’s cells, compared to injecting the gene vector intravenously or via a lumbar puncture. Since higher concentrations of vector can be toxic and manufacturing the vectors is very expensive, the suboccipital puncture has become the desired approach for gene delivery. Some early clinical trials employed an open surgical approach to access the brain, but open surgical procedures come with certain risks and recovery time. The suboccipital puncture — a simpler, needle-based procedure, was, perhaps, a better way after all.
So Pukenas, an assistant professor, and several of his colleagues in Radiology, brushed up on that old procedure. But Pukenas kept thinking about it. It wasn’t a perfect solution.
“The underlying burning question in my head was scalability,” Pukenas said. “If you read the gene therapy trials, people are trying to cure a lot of diseases, including big ones like Parkinson’s and Alzheimer’s, all with gene therapy. If you think about just Phase 1 trials for Parkinson’s, that may be 200 people. Once these trials move to Phase 3 and become part of the clinical practice, there just won’t be enough people to deliver these life-changing therapies with the suboccipital puncture.”
But, what if there were a new and even better way?
That’s when Pukenas became an inventor of something new.
Cameras had become tiny enough that Pukenas speculated he could attach a camera to a catheter to help safely guide it up the spinal canal from the lower back to the brain stem, in real time, without hitting nerves. “The reason you can do that is because the CSF, the fluid that surrounds the spine and the brain, is clear,” Pukenas said. “It’s just like swimming in a pool with goggles on.”
Armed with the realization that this idea could, hypothetically, work, Pukenas submitted a simple sketch and description to the Penn Medicine Medical Device Accelerator program. Since he was accepted into the 2018 class, his idea has made rapid progress toward becoming a practical tool in physicians’ arsenals — perhaps in very many of them, and not too far in the future.
The Medical Device Accelerator Program is part of the Penn Medicine Center for Health Care Innovation, and it offers to help participants “turn science fiction into science.” Penn inventors accepted into the program receive seed funding and project support to help them find collaborators inside and outside of Penn with complementary expertise in disciplines like engineering and product design, develop their idea into a proof of concept and prototyping (often using tools such as 3-D printing), and helps hand them off to the Penn Center for Innovation, whose expertise includes patenting, licensing, and commercialization.
The camera-guided catheter has gone through the first phase of development, which included testing in laboratory models and on a human cadaver. Design modifications are underway now, and Pukenas hopes that the next version will be nearer to ready to use on a living human after the appropriate regulatory approvals. If all of those steps are successful, Pukenas hopes to see clinical trials begin for the catheter potentially within a year.
“It has been an eye opening experience,” Pukenas said of working as part of the device accelerator. “I’m doing things I never thought I’d be doing, like forming a company, and writing a small business grant, it’s all new and exciting and interesting.”
Pukenas has benefitted from the support of Mohit Prajapati, MBA, director of research and development for the Medical Device Accelerator Program, whom he credits as “instrumental” to the progress his invention has made.
“This type of invention is unique to Penn because Penn’s advancement in gene therapy is what really made clear that something like this could be useful,” Prajapati said.
Getting a catheter like this into clinical practice could simplify the delivery of gene therapies to the brain by making the procedure one that many clinicians could do. Lots of physicians are skilled at catheter-based procedures, Pukenas noted, including interventional radiologists, neurosurgeons, and neurologists.
Plus, down the line, such a catheter could open up new possibilities.
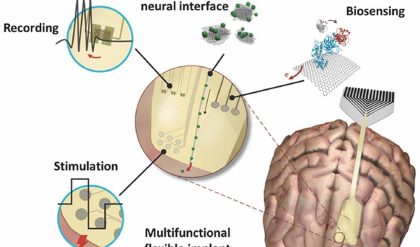
“Once you’re in that space, you’ve bypassed the blood-brain barrier, you have free rein to perform other kinds of procedures,” Pukenas noted. These could include more closely monitoring epilepsy with implantable electrodes, intervening on aneurysms, or delivering highly localized chemotherapy to a brain tumor. “For pretty much anything that involves open brain surgery, we’re trying to come up with ideas to do it using this catheter,” he said.