Spinal cord injury, any of various conditions caused by damage to the tract of nerves that extends from the base of the brain through the canal of the spinal column. Spinal cord injury often has permanent consequences for the function of body parts below the site of injury, the extent of which depends on whether the injury is incomplete, leaving some degree of sensation and movement, or complete, resulting in paralysis.
Causes and Levels Of Spinal Cord Injury
The most dramatic cause of spinal cord injury is acute trauma, such as from motor vehicle accidents, sports accidents, accidental falls, and violence (e.g., gunshot and stab wounds). However, chronic trauma, such as from herniated intervertebral disks or primary or secondary tumours, and injury sustained as a result of certain medical conditions, such as interrupted blood flow to the spinal cord from anterior spinal artery syndrome, can also severely compromise spinal cord function.
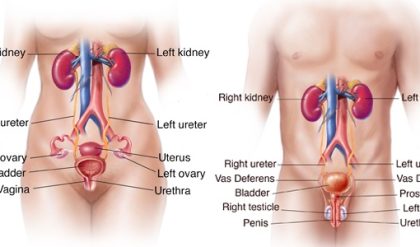
Spinal cord injuries typically are distinguished by the level of injury within the spinal column, whether it occurs at vertebrae in the cervical, thoracic, lumbar, or sacral region. Thus, cervical injuries can occur at levels C1–C8, thoracic injuries at levels T1–T12, lumbar injuries at L1–L5, and sacral injuries at S1–S5. Cervical spinal cord injuries typically result in quadriplegia (or tetraplegia), because they cause weakness or paralysis in the arms and legs. Thoracic, lumbar, and sacral spinal cord injuries may result in paraplegia (weakness or paralysis in the legs) and cause dysfunction of the bladder, bowel, and sexual organs.
Epidemiology Of Spinal Cord Injury
Estimates on the incidence of spinal cord injury vary, depending on country and mode of reporting. The annual global incident rate of spinal cord injury ranges from 15 to 40 cases for every one million people. According to estimates by the Canadian Paraplegic Association, about 35 new cases per million population are seen each year in Canada. Of the 12,000 new cases of paraplegia and quadriplegia that occur in the United States each year, 4,000 patients die before reaching the hospital. Men are afflicted four times as often as women, and about 50 percent of the injury victims are between ages 16 and 30.
A loss of physical function can have an impact on the ability of persons to achieve economic independence following spinal cord injury. Individuals may also experience limitations in their ability to participate in social activities, because of architectural barriers (e.g., buildings accessible by stairs only) and barriers created by negative or overprotective attitudes of healthy, noninjured people toward persons with spinal cord injury. Where social reintegration of young spinal cord injury victims cannot be achieved, both the victim and society suffer; the former is prevented from enriching his life through social interactions, and the latter loses that person’s contributions and incurs heavy expenses associated with the person’s lifelong care.
Changing Attitudes And Therapeutic Approaches
The first known description of acute spinal cord trauma and resulting neurological deficits was found in the Edwin Smith papyrus, a medical treatise thought to be a copy of a work dating to c. 3000 BCE. In the treatise, typical conditions encountered in medical practice were presented as case descriptions, and advice regarding treatment was offered. According to the papyrus, spinal cord injury was “an ailment not to be treated.” That was possibly an expression of helplessness on the side of the medical profession at the time. A doctor’s value would be measured by the extent of cure achieved. Since no strategies that ensured long-term survival for patients with spinal cord injury existed, the doctor would waste time and effort and endanger his reputation. That basic attitude toward victims of spinal cord injury lasted into the 20th century.
In the Balkan Wars (1912–13), there was a 95 percent mortality rate for patients with spinal cord injury, and in World War I (1914–18), about 80 percent of American soldiers with spinal cord injury died before they returned home. During World War II (1939–45), however, the survival rate of soldiers with spinal cord injuries increased dramatically; 20 years after the war, some 75 percent of paraplegics were still alive. Specialized hospital units known as peripheral nerve centres, which had been developed in the time between the two World Wars, demonstrated the advantages of delivering tailored care to special-needs patients. Great importance was attributed to the unique opportunities offered by such specialized units, particularly their ability to offer new insight into the natural course of spinal cord injury and to further the development of new therapeutic strategies.
Building on those experiences, several specialized spinal cord units were opened throughout England in the 1940s. The team of German British neurologist Sir Ludwig Guttmann at the Spinal Unit of the Stoke Mandeville Hospital in Buckinghamshire pioneered new treatment approaches, including frequent repositioning of paralyzed patients to avoid the development of bedsores as a potential source of sepsis and intermittent sterile catheterization to prevent urinary sepsis. The success, measured in patient survival, was dramatic enough to require the development of completely new strategies for social reintegration of patients with spinal cord injury.
Guttmann and colleagues viewed physical rehabilitation as the basis of social reintegration, both physically and psychologically, and they supported the idea of athletic competition in disciplines adequate and adapted to the physical capacity of their patients. Starting with a two-team competition in 1948, paralleling the Olympic Games in England, the idea of competitive sports for the paralyzed developed rapidly. In 1960 the first Paralympic Games were held in Rome. At the same time, the creation of adapted workplaces and wheelchair-accessible housing became an integral component in the framework of social politics in most industrialized countries. Advances in the treatment of spinal cord injury continued in the late 20th and early 21st centuries, such that respiratory complications, heart disease, septicemia, pulmonary emboli, suicide, and unintentional injuries became the major causes of death in patients with spinal cord injury.
Initiatives And Public Awareness
A number of initiatives intended to decrease the incidence of spinal cord trauma and to lend support and advice to patients with spinal cord injuries and their families have been developed at communal and national levels in many countries. Some also offer financial support for basic science and clinical research. Among organizations active in the early 21st century, the prevention-oriented ThinkFirst initiative, the Canadian-based Wheels in Motion, the Christopher & Dana Reeve Foundation, the London Spinal Cord Injury Centre, and the Paralyzed Veterans of America all aimed to increase public awareness and improve treatment for spinal cord injury.
Prevention plays a major role in decreasing the incidence and severity of spinal cord injury. Improvements in prehospital care, including widespread instruction in the principles of first aid and introduction of the principle of spinal cord immobilization during rescue and transport, could help to reduce additional injury sustained after initial trauma. Increased public awareness of risk factors leading to head trauma and spinal cord injury, the introduction of the mandatory use of safety belts, and the installation of air bags in cars also aimed at decreasing trauma severity.
Spinal Cord Injury Research
For many decades it was assumed that once spinal cord trauma had occurred, damage to the central nervous system (CNS) was permanent and repair impossible. At the beginning of the 21st century, that dogma ceased to exist in the minds of scientists, clinicians, and patients and their families. In laboratories worldwide, research became focused on two general approaches: prevention of secondary injury and repair of manifest damage. The term secondary injury is used to describe the observation that CNS structures, which have survived the primary mechanical trauma, die at a later time point because of deterioration of the milieu at the site of injury. The volume of secondary tissue injury can be significantly larger than that caused by the primary injury. Thus, the identification of substances and therapeutic methods that help to minimize secondary injury could improve overall outcome from spinal cord injury. The study, isolation, and manipulation of specific cell types have helped advance research aimed at the repair of injury. Of particular promise in that regard are stem cells, which could help repair damaged CNS structures.
Clinical research on spinal cord injury in the 21st century focused on physical mobilization and on ameliorating the consequences of injury, such as through the identification of stimulators for bladder control and the development of orthopedic correctional procedures. Integration of biomedical research, such as research on pattern generators and on the mechanics and kinetics of movement, with the latest developments in computer science and engineering has improved scientists’ understanding of neural networks and functional control in the CNS. On the basis of that advance, researchers made significant progress toward the development of neuroprostheses, which harness electrical currents to help restore function in persons with nerve damage.