I really enjoy studying biomechanics. I find it totally fascinating to learn, for example, that a certain muscle is very well suited to stabilize a joint, but not to move it through a large range of motion; or that it is active in one movement but not another; or that it becomes atrophied in people with chronic pain. I think this kind of detective work is very cool and I always look forward to applying it to help one of my clients. But that is where things get frustrating, because with biomechanics, as with so many other subjects, the more you learn, the more you realize you don’t know as much as you would like to know. And sometimes you don’t know enough for your treatment protocols to make any sense.
Following are a few random observations that remind me that manual therapists such as myself need to stay humble about the extent of our biomechanical knowledge.
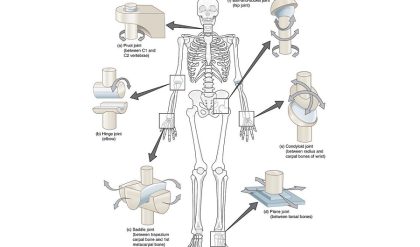
Joints Interactions are Complex
I recently picked up a very intensely biomechanical book called Human Locomotion by Thomas Michaud. Very cool book! And humbling. This book is about four hundred pages of detailed biomechanics analysis, most of which you need about two advanced degrees to understand and apply.
One takeaway that I received from browsing through this book is that different people have different bony shapes, the differences are hard to detect, and these differences have important biomechanical consequences. For example, the book is literally filled with passages like the following:
The subtalar joint motion may be limited by bony restrictions that block pronation and/or supination. The most common bony restriction that limits supination is the tri-articulated subtalar joint. This anomaly occurs in approximately 36% of the population and produces a restriction that prevents continued subtalar joint supination when the anterolateral facets of the calcaneus contacts the anterolateral facet of the talus.
…
Another example of a bony restriction that limits the range of subtalar joint supination is the rudimentary talocalcaneal bridge. … This bony anomaly, which is very difficult to identify with conventional x-ray techniques, acts as an osseous block that maintains the heel in an everted position.
Another interesting takeaway from this book is that expert opinion about even simple biomechanics can be completely overturned by new technologies that provide better measurements. For example, recent 3-D imaging techniques to determine the effects of orthotics on gait revealed findings that were totally surprising to orthotics experts, including that it is far harder to prevent pronation with an orthotic than was previously thought.
Muscles are (surprisingly) complex
We all know the function of a multi-joint structure like the foot is complex, but even the simple actions of a muscle can be very hard to determine. I have recently come across at least three examples of how common assumptions about muscle function have been challenged by research.
The psoas
We are still learning about the basic function of the psoas, and debate continues, even amongst the foremost experts in the world. But there is growing evidence that it functions more as a spinal stabilizer and hip stabilizer than a hip flexor, and that it works to create posterior pelvic tilt as opposed to anterior tilt during standing. This information clearly calls into question the biomechanical rationale of “releasing” the psoas to help with back pain supposedly caused by anterior pelvic tilt or hyperlordosis.
The upper trapezius
Research by Bogduk argues that the upper trap serves more to stabilize and retract the scapula than to elevate it and upwardly rotate it. This calls into question the biomechanical rationale of many treatments of upper cross syndrome.
The supraspinatus
We are all taught that the supraspinatus initiates abduction of the shoulder, but new research indicates that it does not activate any earlier than the deltoid. Perhaps this has implications for the biomechanical rationale underlying treatments for shoulder impingement.
The point here is not so much to argue in favor of any of the new interpretations offered in the above research, but to simply note that some very basic biomechanical issues have not yet been settled, and that many treatment protocols may be proceeding on a faulty base of unsupported assumptions.
Complexity makes prediction difficult in the presence of error
One of the simplest models that drives a great many treatments in manual therapy is based on the lower cross syndrome. For example, a client comes in with lower back pain, and assessment reveals that the client’s pelvis is anteriorly tilted and the lumbar spine is hyperlordotic. The therapist decides that the psoas is “short” and needs to be lengthened or released.
Now this is about as simple as any biomechanically based treatment gets in manual therapy, but let’s look at how many things would need to be true for this story to make sense. There are many links in the chain of reasoning, and regular readers will immediately notice that almost all of them are flawed.
First, there is very little reason to believe that low back pain is caused by excess lumbar lordosis or anterior pelvic tilt, because most studies find very little correlation between these variables.
Second, given considerable individual anatomical variation in vertebral shape, sacral base angle and bony landmarks on the pelvis, we have reason to question someone’s ability to assess that a particular client is standing in anterior tilt or hyperlordosis, as opposed to a posture that is neutral for their particular structure.
Third, as we just learned about the psoas, it might play no role in increasing anterior pelvic tilt in standing, and in fact might even perform the opposite function.
Fourth, there is little reason to believe that manual therapy could lengthen a short psoas.
So the chain of reasoning does not hold up in any of its links, much less all of them.
And this is one of the simplest biomechanical models that we see, one that is taught to novices. More sophisticated biomechanical models, that people may study for years, often have even more links in the chain of reasoning, creating even more places to go wrong. For example, overactivity of muscle A in the pelvis inhibits the activity of muscle B, which moves joint C into flexion, which causes joint D to compensate by moving into extension, which eventually brings us to . . . the lateral pterygoid! Each successive link in the chain makes it far more likely for error to be introduced. And errors are particularly problematic in a complex system.
One of the characteristics of a complex system is that you cannot predict its behavior unless you have perfect knowledge of all the variables and how they interact. Even very small errors in measurement of the initial conditions of the system will lead to huge errors in prediction after a little time passes. Therefore, to the extent that the body’s interactions are complex, which they often are, it is unlikely that we can predict how changes in one area will affect a distant area. We might be confident that one will affect the other, but exactly how might be very hard to determine.